Athlete's Foot
Seeking professional medical advice for athlete's foot is essential for an accurate diagnosis and appropriate treatment. The dermatologists at Dermatology Affiliates can provide personalized care to address your specific concerns.
Examples of Athlete's foot


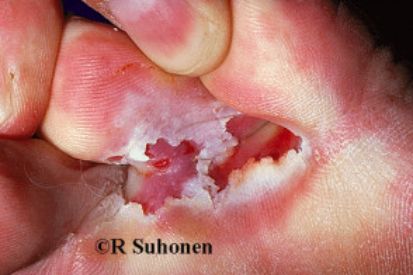

Symptoms of Athlete's Foot
- Itching, stinging, and burning sensations, particularly between the toes and on the soles of the feet.
- Blisters on the feet, contributing to heightened discomfort and a potential source of infection.
- Cracking and peeling of skin.
- Infected nails may exhibit discoloration, often appearing thickened and crumbly.
- As the infection progresses, individuals may also experience a foul odor emanating from the affected feet.
Causes of Athlete's Foot
- Athlete's Foot is primarily caused by fungal infections.
- These fungi thrive in warm, damp environments like locker rooms, communal showers, and swimming pool areas.
- Highly contagious and spreads through direct contact with contaminated surfaces or by coming into contact with the skin of an infected person.
- Tight-fitting, non-breathable footwear, and damp socks create an ideal environment for fungal growth.
- Compromised immune systems, excessive sweating, and minor skin injuries increase susceptibility to the infection.
- Walking barefoot in public spaces where the fungus is present.
- Anyone, regardless of activity level, can be affected.
How to Prevent Athlete's Foot
- Wash feet daily with soap and water, ensuring thorough drying, especially between toes.
- Use moisture-wicking socks made of breathable materials like cotton; change them regularly, especially if damp.
- Choose well-ventilated shoes to allow feet to breathe and reduce fungal growth.
- Avoid walking barefoot in public areas, especially in places like locker rooms, communal showers, and swimming pool decks.
- Consider wearing flip-flops or shower shoes in public facilities to protect against direct contact with contaminated surfaces.
- Rotate shoes to allow for adequate air circulation and consider using antifungal powder or spray inside footwear.
- Refrain from sharing personal items like socks, shoes, and towels to prevent the spread of infection.
- Keep toenails trimmed and clean to reduce spaces for fungal growth.
- Use moisture-wicking insoles or antiperspirant powders if prone to excessive sweating.
- Regularly inspect feet for redness, itching, or unusual changes; seek prompt medical attention if Athlete's Foot is suspected.
Athlete's Foot FAQs
A dermatologist can diagnose athlete's foot through a visual examination of the affected skin. To confirm the diagnosis, the dermatologist may also perform a skin scraping for microscopic analysis or send a sample for a fungal culture. Accurate diagnosis is essential for determining the most effective treatment plan for athlete's foot.
Yes, athlete's foot can spread to other areas of the body if preventative measures are not taken. The fungi responsible for athlete's foot flourish in warm, moist environments. The infection could spread to other parts of the body, such as the groin or hands if a person with athlete's foot touches the infected area and then other parts of the body. To prevent this, it's crucial to wash hands thoroughly after touching the affected area and to avoid scratching, which can further spread the fungus.
Yes, athlete's foot can return, usually if preventive measures are ignored or if the conditions that caused the infection are not corrected. To reduce the risk of recurrence, it's crucial to complete the entire course of prescribed antifungal treatment, maintain excellent foot hygiene, keep feet dry, and avoid environments where the fungus can flourish, such as public pools or shared showers. Regular monitoring and proactive steps can further help prevent future infections.
Yes, consulting a dermatologist for athlete's foot is recommended if over-the-counter treatments fail or if the condition is severe or recurring. A dermatologist can provide a precise diagnosis and prescribe effective treatments tailored to your needs. They can also offer advice on preventing future infections and managing the condition effectively, ensuring proper treatment and quicker recovery.
How to Treat Athlete's Foot
In some cases, Athlete’s Foot can be treated with over-the-counter antifungal creams, ointments, or sprays containing active ingredients like terbinafine, clotrimazole, or miconazole that can be applied to the affected area.
However, it is recommended you consult a dermatologist. They can create a thorough evaluation and personalized treatment plan that may include prescribing stronger topical or oral antifungal medications to combat the infection more effectively. It is best to avoid irritants and keep your feet dry to limit the spread of infection.
By combining these measures, individuals can effectively manage and eliminate Athlete's Foot while minimizing the risk of recurrence.
Featured Blogs

- General Dermatology
- Skin Care
- Chronic Skin Conditions
Skin tags are benign growths of excess skin which form in response to rubbing and irritation. Read more to learn about what we can do about them.
Read More
- Skin Care
- Cosmetic Treatments
I had my second Elos Sublative RF Microneedling Treatment (which is an amazing new treatment we’ve added for addressing fine lines, wrinkles, acne scars and texture).
Read More
- Skin Care
- Botox
- Cosmetic Treatments
Retiniods are proven to combat fine lines, brown spots and improve texture, “tret” has been shown to enhance collagen production, even skin tone, unclog pores, and smooth skin texture.
Read MoreFeatured Products
Check your local office for current stock!
Check your local office for current stock!
