Molluscum
At Dermatology Affiliates, our expert team is well-versed in molluscum contagiosum management, commonly addressing the face, neck, arms, and genital areas. If you're dealing with these characteristic lesions, our trusted Dermatology Affiliates providers offer specialized care and advanced treatments to effectively address and eliminate molluscum contagiosum. Schedule an appointment at Dermatology Affiliates for a thorough evaluation and tailored treatment plan to prevent further spread and restore skin health.
Examples of Molluscum




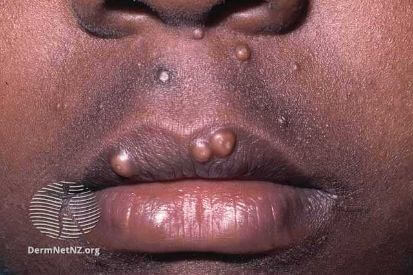
What are the Symptoms of Molluscum?
- Appearance: Smooth, pearly, flesh-colored skin growths.
- Initiation: Begin as small bumps, potentially growing as large as a pencil eraser.
- Central Pit: Many lesions feature a central pit housing the virus bodies.
- Itching: Molluscum is typically accompanied by itching.
- Skin Infection: Surrounding skin may become infected due to the growths.
- Duration: Bumps can persist for two weeks to one and a half years.
- Self-Resolution: Lesions may resolve spontaneously.
Causes of Molluscum
- Molluscum contagiosum virus (MCV).
- This viral skin infection primarily affects humans, leading to the formation of characteristic skin lesions.
- Transmission occurs through direct skin-to-skin contact with an infected person.
- Contact with contaminated objects such as towels or toys.
How to Prevent Molluscum
- Hand Hygiene: Regular handwashing with soap and water can help reduce the risk of spreading and contracting the virus.
- Avoiding Direct Contact: Minimize skin-to-skin contact, especially with individuals who have active molluscum lesions. This is particularly important in communal settings such as schools and sports facilities.
- Personal Items: Refrain from sharing personal items like towels, clothing, and toys, which could potentially carry the virus from one person to another.
- Avoid Scratching: Discourage excessive scratching of existing lesions, as this can rupture the lesions and facilitate the virus's spread.
- Environmental Cleanliness: Maintain cleanliness in shared spaces, including sports equipment, gym facilities, and communal bathing areas.
Molluscum FAQs
To diagnose molluscum contagiosum, your dermatologist will typically examine the distinctive bumps on your skin. Occasionally, they may take a small sample for further analysis. The process is generally quick and straightforward, allowing for accurate confirmation of the condition.
It is reccomended to visit your dermatologist for individualized advice and treatment. Over-the-counter treatments may not be the most effective, and your dermatologist can suggest the safest and most appropriate options tailored to your individual needs.
Yes, molluscum bumps can spread to other parts of your body. Since they are contagious, touching or scratching them can cause them to appear elsewhere on your skin. To prevent this, avoid picking at the bumps and wash your hands frequently.
Typically, people with molluscum can carry on with their usual activities, such as going to school or work. However, it's important to avoid sharing personal items and maintain good hygiene to minimize the risk of spreading the infection to others.
In most instances, molluscum lesions typically do not result in lasting scars. Yet the risk of scarring may increase if the bumps are scratched or picked at. Dermatologists can offer guidance on reducing the likelihood of scarring and maintaining healthy skin throughout and after the infection.
How to Treat Molluscum
- Cantharone, a blistering agent made from beetles, is applied with a wooden applicator to the skin growth. The medicine should be washed off in 4 to 6 hours. A small blister usually forms in a few hours to one day. When the scab falls off, the growth is gone. The application of this treatment is not painful; it is used on the face and in skin creases. Scarring does not occur from Cantharone treatment. Although blisters are uncomfortable, they are very superficial and resolve within a few days.
- Freezing with liquid nitrogen is another form of treatment. Liquid nitrogen is applied with a cotton-tipped applicator, feels hot for a moment, and then may form a blister or irritation at the site.
- Another way to remove molluscum is by scraping the bump or removing the center, a treatment that is performed after numbing the area with a special cream.
Featured Blogs

- General Dermatology
- Skin Care
- Chronic Skin Conditions
Skin tags are benign growths of excess skin which form in response to rubbing and irritation. Read more to learn about what we can do about them.
Read More
- Skin Care
- Botox
- Cosmetic Treatments
Bridal prep is very extensive. There’s the dress, food, makeup, decor, guest list and of course the beauty routine for the bride. Read more to learn how we can help you get glowing skin.
Read More
- Skin Care
- Cosmetic Treatments
I had my second Elos Sublative RF Microneedling Treatment (which is an amazing new treatment we’ve added for addressing fine lines, wrinkles, acne scars and texture).
Read MoreFeatured Products
Check your local office for current stock!
Check your local office for current stock!
